Patient Information
PURIXAN® (pure-ee-zan)
(mercaptopurine) oral suspension 20 mg/mL
What is PURIXAN?
PURIXAN is a prescription medicine used along with other medicines to treat people with acute lymphoblastic leukemia (ALL).
What should I tell my healthcare provider before taking PURIXAN?
Before you take PURIXAN, tell your healthcare provider about all of your medical conditions, including if you:
- have kidney or liver problems.
- have a condition where your body produces too little of the enzyme thiopurine methyltransferase (TPMT) or the enzyme nucleotide diphosphatase (NUDT15).
- have recently received or plan to receive a vaccine.
- are pregnant or plan to become pregnant. PURIXAN can harm your unborn baby.
If you are a female who is able to become pregnant:- Your healthcare provider will do a pregnancy test before you start treatment with PURIXAN.
- Use an effective method of birth control (contraception) during treatment with PURIXAN and for 6 months after your last dose. Talk with your healthcare provider about birth control methods you can use during this time.
- Tell your healthcare provider right away if you become pregnant or think you are pregnant during treatment with PURIXAN.
If you are a male with a female partner who is able to become pregnant:
- Use effective birth control (contraception) during treatment with PURIXAN and for 3 months after your last dose.
- Tell your healthcare provider right away if your female partner becomes pregnant or thinks she is pregnant during your treatment with PURIXAN.
- are breastfeeding or plan to breastfeed. Do not breastfeed during treatment with PURIXAN and for at least 1 week after your last dose.
- Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
How should I take PURIXAN?
- See the detailed “Instructions for Use” that comes with PURIXAN for information about the right way to measure and take a dose of PURIXAN.
- Take PURIXAN exactly as your healthcare provider tells you. Do not stop taking PURIXAN or change your dose without talking to your healthcare provider.
- Take PURIXAN by mouth 1 time each day.
- If PURIXAN comes into contact with skin, eyes, or clothes?
- Remove contaminated clothing.
- Wash skin or eyes immediately with water.
- Contact with skin or eyes can cause hypersensitive reactions resulting in rash, redness, itching and inflammation. If symptoms appear seek medical attention.
- During treatment with PURIXAN, your healthcare provider will do blood tests regularly to check your blood cell counts and liver function. Your healthcare provider may change your dose if you have side effects.
- If you miss a dose of PURIXAN, call your healthcare provider for advice.
- If you take too much PURIXAN, call your healthcare provider or go to the nearest emergency room right away.
What should I avoid while taking PURIXAN?
PURIXAN can make your skin more sensitive to sunlight. Protect yourself from sunlight during treatment with PURIXAN.
What are the possible side effects of PURIXAN?
PURIXAN can cause serious side effects, including:
- Decreased blood cell counts are common with PURIXAN, but can also be severe. PURIXAN affects your bone marrow and can cause decreased white blood cells, red blood cells, and platelets. Decreased blood cell counts can make you more likely to develop infections, bleeding, or anemia. If you take certain medicines during treatment with PURIXAN, it could make the effects on your bone marrow worse. Tell your healthcare provider if you develop any of the following symptoms during treatment with PURIXAN:
- fever
- sore throat
- cuts or wounds that are red, or swollen, or are draining
- any bleeding
- tiredness or weakness
- shortness of breath
- Liver problems. Increases in liver function test results are common with PURIXAN, but you can also develop severe liver problems with PURIXAN that can lead to death. Your healthcare provider may tell you to stop taking PURIXAN if you develop liver problems. Tell your healthcare provider right away if you develop any of the following symptoms of a liver problem during treatment with PURIXAN:
- decreased appetite
- diarrhea
- nausea or vomiting
- yellowing of your skin or the whites of your eyes
- a build-up of fluid in your stomach-area (ascites)
- Possible increased risk of other cancers. Talk with your healthcare provider about your risk of other cancers if you take PURIXAN.
Less common side effects of PURIXAN include: loss of appetite, nausea, vomiting, diarrhea, generally do not feel well, and rash.
Low blood sugar (hypoglycemia) can happen, especially in children under six years of age.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of PURIXAN.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store PURIXAN?
- PURIXAN comes in a bottle with a child-resistant cap.
- Store PURIXAN between 59ºF to 77ºF (15ºC to 25ºC), in a dry place. Do not store above 25°C.
- Store the oral dispensing syringe in a clean place, with the medicine.
- PURIXAN oral suspension should be used within 8 weeks after opening the bottle. Dispose of (throw away) any unused medicine after 8 weeks.
- Do not use after the expiry date which is stated on the carton and the bottle after ‘EXP’.
- Keep the bottle tightly closed to prevent spoilage of the medicine and reduce the risk of accidental spillage.
- Keep PURIXAN out of the reach of children, preferably in a locked cupboard. If a child accidentally takes PURIXAN, it could cause death.
How should I dispose of PURIXAN?
- This medicine should not be disposed of in wastewater or household waste. Ask your pharmacist how to dispose of (throw away) PURIXAN that is no longer needed.
General information about the safe and effective use of PURIXAN.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use PURIXAN for a condition for which it was not prescribed. Do not give PURIXAN to other people, even if they have the same symptoms you have. It could harm them. You can ask your healthcare provider or pharmacist for information about PURIXAN that is written for health professionals.
What are the ingredients in PURIXAN?
Active ingredient: mercaptopurine
Inactive ingredients: xanthan gum, aspartame, concentrated raspberry juice, sucrose, ethyl parahydroxybenzoate sodium, methyl parahydroxybenzoate sodium, potassium sorbate, sodium hydroxide and purified water.
Manufactured by: Nova Laboratories Ltd, Leicester, LE18 4YL, United Kingdom
Manufactured for: Rare Disease Therapeutics, Inc., 2550 Meridian Blvd. Suite 150, Franklin, TN 37067
For more information, go to www.purixan-us.com.
This Patient Information has been approved by the U.S. Food and Drug Administration
Revised: April 2020
Part Number: D001113/1
Instructions for Use
PURIXAN® (pure-ee-zan)
(mercaptopurine) oral suspension 20 mg/mL
Read these Instructions for Use before you start taking PURIXAN, and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
Important information about measuring PURIXAN oral suspension
- Always use the oral dispensing syringe provided with your PURIXAN oral suspension to make sure you measure the right amount.
- You will be provided:
- 1 bottle of PURIXAN oral suspension
- 1 bottle adapter
- 2 oral dispensing syringes (one 1 mL and one 5 mL)
If you did not receive an oral dispensing syringe with your PURIXAN oral suspension, ask your pharmacist to give you one.
You will also need disposable gloves.
Important Information You Need to Know Before Administering PURIXAN:
- Wash your hands well with soap and water before and after administering a dose.
- Put on disposable gloves before handling PURIXAN.
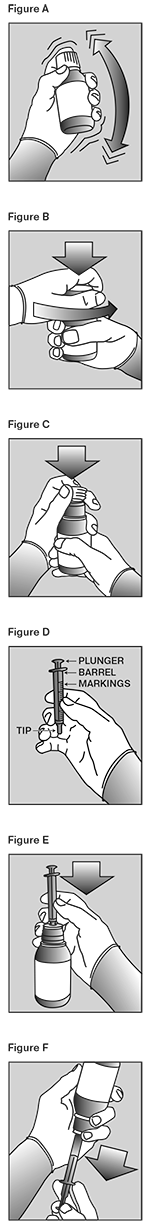
- Shake the bottle vigorously for at least 30 seconds to make sure that the medicine is well mixed (See Figure A).
- Remove the child-resistant bottle cap (see Figure B).
- Push the ribbed end of the bottle adapter into the neck of the bottle until it is firmly in place. The bottom edge of the adapter should fully contact the top rim of the bottle (See Figure C). Do not remove the adapter from the bottle after it is inserted.
Preparing a dose of PURIXAN:
- Hold the bottle upright. Remove the bottle cap by turning in the direction of the arrow (See Figure B).
- Push the tip of the oral dispensing syringe into the hole in the bottle adapter (See Figure D and Figure E).
- Turn the bottle upside down (See Figure F).
- Pull back slowly on the plunger of the oral dispensing syringe to withdraw the prescribed dose of PURIXAN. Pull the plunger back to the mL mark on the syringe that corresponds to the dose prescribed (Figure F). If you are not sure about how much medicine to draw into the oral dispensing syringe, always ask your doctor, pharmacist or nurse for advice.
- Leave the oral dispensing syringe in the bottle adapter and turn the bottle right-side up. Place the bottle onto a flat surface. Hold the oral dispensing syringe by the barrel and carefully remove it from the adapter. Do not hold the oral dispensing syringe by the plunger, because the plunger may come out.
- Place the tip of the oral dispensing syringe in your mouth and aim the tip toward the inside of your cheek.
- Gently squirt the PURIXAN oral suspension into your mouth by pushing on the plunger until the oral dispensing syringe is empty. Swallow the medicine.
- Do not forcefully push on the plunger.
- Do not squirt the medicine to the back of your mouth or throat. This may cause you to choke.
- Remove the oral dispensing syringe from your mouth.
- Swallow the dose of oral suspension then drink some water, making sure no medicine is left in your mouth.
- Put the cap back on the bottle with the adapter left in place. Close the cap tightly.
- Wash the oral dispensing syringe with warm soapy water and rinse well. Hold the oral dispensing syringe under water and move the plunger up and down several times to make sure the inside of the oral dispensing syringe is clean. Let the oral dispensing syringe dry completely before you use it again for
dosing. Do not throw away the oral dispensing syringe after use.
Ingredients in PURIXAN
Active ingredient: mercaptopurine
Inactive ingredients: xanthan gum, aspartame, concentrated raspberry juice, sucrose, ethyl
parahydroxybenzoate sodium, methyl parahydroxybenzoate sodium, potassium sorbate, sodium hydroxide, and purified water.
Storing PURIXAN
- Store PURIXAN between 59ºF to 77ºF (15ºC to 25ºC), in a dry place. Do not store above 25°C.
- Store the oral dispensing syringe in a clean place, with the medicine.
- PURIXAN oral suspension should be used within 8 weeks after opening the bottle. Dispose of (throw away) any unused medicine after 8 weeks.
- Do not use after the expiry date which is stated on the carton and the bottle after ‘EXP’.
- Keep the bottle tightly closed to prevent spoilage of the medicine and reduce the risk of accidental spillage.
- Keep PURIXAN oral suspension and all medicines out of the reach of children, preferably in a locked cupboard. If a child accidentally takes PURIXAN, it could cause death. Ask your pharmacist how to dispose of (throw away) PURIXAN that is no longer needed.
Disposing of PURIXAN
- Ask your pharmacist how to dispose of PURIXAN that is expired or no longer required. Medicines should not be disposed of via wastewater or household waste.
Clean Up Spillage of PURIXAN
Use appropriate personal protective equipment (disposable gloves and eye protection). Mop up and contain spill material in a compatible container. Wash your hands thoroughly afterwards.
PURIXAN Contact with Skin, Eyes, or Clothes
- Remove and launder contaminated clothing.
- Wash skin or eyes immediately with water.
Contact with skin or eyes can cause hypersensitive reactions resulting in rash, redness, itching and inflammation. If symptoms appear, seek medical attention.